Kim Novak diagnosed with Breast Cancer

Actress Kim Novak has been diagnosed with breast cancer. The 77-year-old, best known for her starring role again Carey Grant in Hitchcock’s thriller Vertigo, was reportedly diagnosed after a routine yearly mammogram and is currently undergoing treatment. Her manager, Sue Cameron is quoted as saying: “All her doctors say she is in fantastic physical shape and should recover very well.”
We have already discussed breast cancer in several blogs, as well as the current recommendations for mammograms. Today, I thought we would touch on some basics about mammograms.
What is a mammogram? Source: National Cancer Institute
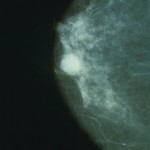
A mammogram is an x-ray picture of the breast.
Mammograms can be used to check for breast cancer in women who have no signs or symptoms of the disease. This type of mammogram is called a screening mammogram. Screening mammograms usually involve two x-ray pictures, or images, of each breast. The x-ray images make it possible to detect tumors that cannot be felt. Screening mammograms can also find microcalcifications (tiny deposits of calcium) that sometimes indicate the presence of breast cancer.
Mammograms can also be used to check for breast cancer after a lump or other sign or symptom of the disease has been found. This type of mammogram is called a diagnostic mammogram. Signs of breast cancer may include pain, skin thickening, nipple discharge, or a change in breast size or shape; however, these signs may also be indicators of benign conditions. A diagnostic mammogram can also be used to evaluate changes found during a screening mammogram or to view breast tissue when it is difficult to obtain a screening mammogram because of special circumstances, such as the presence of breast implants.
 How are screening and diagnostic mammograms different?
How are screening and diagnostic mammograms different?
Diagnostic mammography takes longer than screening mammography because more x-rays are needed to obtain views of the breast from several angles. The technician may magnify a suspicious area to produce a detailed picture that can help the doctor make an accurate diagnosis.
What are the benefits of screening mammograms?
Early detection of breast cancer with screening mammography means that treatment can be started earlier in the course of the disease, possibly before it has spread. Results from randomized clinical trials and other studies show that screening mammography can help reduce the number of deaths from breast cancer among women ages 40 to 74, especially for those over age 50. However, studies conducted to date have not shown a benefit from regular screening mammography in women under age 40 or from baseline screening mammograms (mammograms used for comparison) taken before age 40.
What are some of the potential harms of screening mammograms?
- Finding cancer does not always mean saving lives―Even though mammograms can detect malignant tumors that cannot be felt, treating a small tumor does not always mean that a woman’s life will be saved. A fast-growing or aggressive cancer may have already spread to other parts of the body before it is detected. In addition, screening mammograms may not help a woman who is suffering from other, more life-threatening health conditions.
- False-negative results―False-negative results occur when mammograms appear normal even though breast cancer is present. Overall, screening mammograms miss up to 20 percent of breast cancers that are present at the time of screening.
 The main cause of false-negative results is high breast density. Breasts contain both dense tissue (i.e., glandular tissue and connective tissue, together known as fibroglandular tissue) and fatty tissue. Fatty tissue appears dark on a mammogram, whereas dense tissue and tumors appear as white areas. Because fibroglandular tissue and tumors have similar density, tumors can be harder to detect in women with denser breasts.False-negative results occur more often among younger women than among older women because younger women are more likely to have dense breasts. As a woman ages, her breasts usually become more fatty, and false-negative results become less likely. False-negative results can lead to delays in treatment and a false sense of security for affected women.
The main cause of false-negative results is high breast density. Breasts contain both dense tissue (i.e., glandular tissue and connective tissue, together known as fibroglandular tissue) and fatty tissue. Fatty tissue appears dark on a mammogram, whereas dense tissue and tumors appear as white areas. Because fibroglandular tissue and tumors have similar density, tumors can be harder to detect in women with denser breasts.False-negative results occur more often among younger women than among older women because younger women are more likely to have dense breasts. As a woman ages, her breasts usually become more fatty, and false-negative results become less likely. False-negative results can lead to delays in treatment and a false sense of security for affected women. - False-positive results―False-positive results occur when radiologists decide mammograms are abnormal but no cancer is actually present. All abnormal mammograms should be followed up with additional testing (diagnostic mammograms, ultrasound, and/or biopsy) to determine whether cancer is present.False-positive results are more common for younger women, women who have had previous breast biopsies, women with a family history of breast cancer, and women who are taking estrogen (for example, menopausal hormone therapy).False-positive mammogram results can lead to anxiety and other forms of psychological distress in affected women. The additional testing required to rule out cancer can also be costly and time consuming and can cause physical discomfort.
- Overdiagnosis and overtreatment―Screening mammograms can find cancers and cases of ductal carcinoma in situ (DCIS, a noninvasive lesion in which abnormal cells that may become cancerous form in the lining of breast ducts) that need to be treated. However, they can also find cancers and cases of DCIS that will never cause symptoms or threaten a woman’s life, leading to “overdiagnosis” of breast cancer. Treatment of these latter cancers and cases of DCIS is not needed, leading to “overtreatment.” Overtreatment exposes women unnecessarily to the adverse effects associated with cancer therapy.Because doctors cannot currently distinguish cancers and cases of DCIS that need to be treated from those that do not, they are all treated.
- Radiation exposure―Mammograms require very small doses of radiation. The risk of harm from this radiation exposure is low, but repeated x-rays have the potential to cause cancer. The benefits, however, nearly always outweigh the risk.Women should talk with their health care providers about the need for each x-ray. In addition, they should always let their health care provider and the technician know if there is any possibility that they are pregnant.
























0 comments