Def Leppard Guitarist’s Cancer Returns

Many were applauding when Def Leppard guitarist Vivian Campbell announced in November that he was in remission from Hodgkin’s Lymphoma. Campbell, 51, had been diagnosed with the cancer earlier in the year after being evaluated for ‘the cough that wouldn’t quit.'”
Unfortunately, that announcement may have been a bit premature. In an interview with the Utah Daily Herald Campbell said:
“It came right back. I don’t know if the cancer came back or it never totally went away, you know, but the initial scan I did last fall after doing my chemo, the scan came back clean. But there was something about it, the oncologist was unclear about and didn’t feel good about, so I was referred to another specialist.”
A biopsy showed that the cancer had returned.
But Campbell hopes to remain on the road with the band (which is presently touring with KISS) with the help of “high-tech chemo”:
“It’s the first new drug that’s been discovered for Hodgkin’s since 1977 and they made this discovery in 2011, and it’s actually being pioneered here at City of Hope, so I’m part of this research clinical trial that’s going on. It’s very, very benign chemo, actually it just targets — I don’t know how it works… but somehow or other it just manages to target the cancer cells. It’s not like old-school, carpet-bomb chemo where it kills all the fast-growing cells, so I haven’t experienced any hair loss or any issues with my skin or nails or anything this time around, which is good.”
Campbell’s already been through about half of the treatments. If things go well, he will undergo a a stem-cell transplant. Campbell added, “I can’t say I’m looking forward to, but I’ve been told if I don’t do that, the cancer’s going to just keep coming back every couple years. And every time it’s a little bit more resistant. It is what it is. ”
As we do not have access to Campbell’s medical records, we don’t know what specific medication he is on. However, after reviewing the clinical trials currently underway at City of Hope, as well as a recent research literature on Hodgkins Lymphoma, the most likely candidate is a medication called Brentuximab vedotin (trade name: Adcetris). In any case, the drug is one of a number of drugs that are considered Targeted Cancer Therapy- which is becoming the future of cancer treatment.
What is meant by Targeted Cancer Therapy?
 According to the National Cancer Institute targeted cancer therapies are drugs or other substances that block the growth and spread of cancer by interfering with specific molecules needed for tumor growth or spread. Scientists call these molecules “molecular targets.” By focusing on molecular and cellular changes that are specific to cancer, targeted cancer therapies may be more effective than other types of treatment and less harmful to normal cells.
According to the National Cancer Institute targeted cancer therapies are drugs or other substances that block the growth and spread of cancer by interfering with specific molecules needed for tumor growth or spread. Scientists call these molecules “molecular targets.” By focusing on molecular and cellular changes that are specific to cancer, targeted cancer therapies may be more effective than other types of treatment and less harmful to normal cells.
How do cancer cells grow?
In normal cells, growth, division, and differentiation (a process by which a less specialized cell becomes a more specialized cell type) are highly regulated processes. Cells are told what to do by special molecules called signalling molecules. Some of these molecules—called growth factors—tells the cells to divide into more cells. Others cause cells to stop growing or can cause cell death.
Many signaling molecules, including growth factors and growth inhibitors, bind to receptors on the surface of the cell. In many cases, these receptors must interact with one another before they can become fully activated.
Unlike normal cells, cancer cells display uncontrolled growth control- they can ignore signals to stop growing.
Cancer cells use a number of ways to bypass the normal safeguards so they can grow uncontrollably at the expense of normal cells and tissues. These mechanisms include:
Increased signaling for cell growth
Some cancer cells can make their own growth factors. These growth factors travel to the outside of the cell, where they interact with and activate the cancer cell’s growth factor receptors.
Some cancer cells make more growth factor receptors than normal cells—this is called overexpression. Having more receptors available increases the chances that a growth factor will find its receptor.
Evasion of cell death
In adults, the number of body cells is kept relatively constant. Stressed, diseased, malfunctioning, or irreversibly damaged cells, as well as cells that need to be removed routinely as part of normal growth and development, are all removed by a process called apoptosis, also called programmed cell death or cell suicide.
Cancer cells also often avoid cell death by altering the surveillance proteins that normally detect problems.
Other cancer cells evade destruction by overproducing anti-cell death proteins or by creating mutant proteins that are better at blocking cell death signals.
Increased blood vessel formation
The creation of new blood vessels—a highly regulated process called angiogenesis—primarily takes place during early development, when the circulatory system is being formed. In adults, however, angiogenesis normally occurs only to facilitate wound healing or to support various aspects of female reproduction and pregnancy.
Once a tumor gets to a certain size, it requires a blood supply to continue growing. So, tumor cells must find a way to attract new blood vessels. Many tumors release high levels of blood vessel growth factors that bind to and activate the lining cells of nearby blood vessels.
How does Targeted Cancer Therapy work?
Chemotherapy works by stopping or slowing the growth of cancer cells, which grow and divide quickly. But it can also harm healthy cells that divide quickly, which include cells that line your mouth and intestines, cells in your bone marrow that make blood cells, and cells that make your hair grow. Chemotherapy causes side effects (such as hair loss, anemia, sores in the mouth, and nausea) when it harms these healthy cells.
How much better it would be if drug treatment only destroyed cancer cells, and left normal cells alone!
That’s where targeted cancer therapy comes in.
As researchers have learned more details about how different cancers grow, they have uncovered the specific proteins and factors that allow cancer cell growth to go unchecked. Many of these discoveries are the results of DNA sequencing of these cancers.
Unlike traditional chemotherapy, targeted therapies are designed to interact with specific molecules that are part of the pathways and processes used by cancer cells to grow, divide, and spread throughout the body. Targets are chosen very carefully. When researchers discover a potentially vulnerable molecule involved in a cancer process or pathway, they validate it by doing more research, and then, if all goes well, they design new therapies to disrupt its activity with great precision.
Three types of drugs can be used as targeted therapies—small molecule drugs that are taken by mouth, monoclonal antibodies administered by injection, and vaccines.
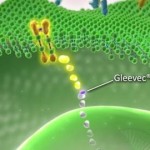 Many targeted therapies are small molecules. Once in the body, most small molecules can easily travel across cell membranes, including the plasma membrane. This means that they can be used to interfere with proteins located either outside or inside the cell. Small molecules are often designed to interact with specific areas of the target protein in order to modify its enzyme activity or its interaction with other molecules.
Many targeted therapies are small molecules. Once in the body, most small molecules can easily travel across cell membranes, including the plasma membrane. This means that they can be used to interfere with proteins located either outside or inside the cell. Small molecules are often designed to interact with specific areas of the target protein in order to modify its enzyme activity or its interaction with other molecules.
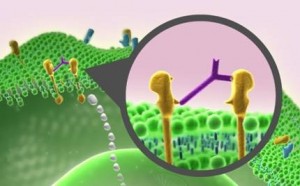
The interaction of signaling molecules with receptors on the outside of a cell often activates pathways inside the cell. Monoclonal antibodies can interfere with these signaling pathways in cancer cells in a number of ways:
First, antibodies can work outside the cell by preventing signaling molecules and receptors from interacting with each other (1).
Second, they can also be used as delivery vehicles, guiding radioactive molecules or toxins to the cancer cells (2).
Third, antibodies attached to a cell can trigger an immune response that destroys the cell (3)
The immune system is programmed to defend the body against invaders, such as a cold virus, but its ability to fight cancer is limited because it doesn’t usually recognize cancer cells as foreign. In fact, some cancers actively suppress the body’s immune responses.Unlike other targeted therapies, therapeutic cancer vaccines do not act specifically on pathways in cancer cells. Instead, they act broadly by trying to activate the body’s immune system to make it recognize and attack cancer cells.
What impact will targeted therapies have on cancer treatment?
Targeted cancer therapies give doctors a better way to tailor cancer treatment, especially when a target is present in some but not all tumors of a particular type. Eventually, treatments may be individualized based on the unique set of molecular targets produced by the patient’s tumor. Targeted cancer therapies also hold the promise of being more selective for cancer cells than normal cells, thus harming fewer normal cells, reducing side effects, and improving quality of life.
Nevertheless, targeted therapies have some limitations. Chief among these is the potential for cells to develop resistance to them. In most cases, another targeted therapy that could overcome this resistance is not available. It is for this reason that targeted therapies may work best in combination, either with other targeted therapies or with more traditional therapies.





























0 comments