Country Singer Joey Feek Passes Away

Joey Martin Feek of the husband/wife country duo Joey + Rory has passed away at the age of 40.
Joey was diagnosed with stage 4 cervical cancer. in 2014, and underwent a radical hysterectomy at that time. In early 2015, doctors told her that her cancer had returned. A 9 cm (3-1/2 inch) tumor was found in her sigmoid colon and the cells in the tumor were the same as the original cancer.
She began chemotherapy and radiation therapy and was scheduled to begin another round of chemotherapy when a CT scan showed “two quarter-sized tumors in the same area they had been blasting daily with chemo and radiation.” Several other spots were also seen throughout her abdomen.
In October Joey and Rory made the difficult decision to stop her treatment. This comes after the singer learned that the treatments she has been undergoing had not stopped the growth of the cancer.
As husband Rory says:
“So we did what you do when the medicine isn’t working, and the doctors are at a loss…and when the ‘statistics” say you can do more chemo, but it will only buy you a little time…
We came home. Not to die. But to live.”
And live she did. Her daily activities were celebrated in a blog created by Rory, The Life I Live. Through the blog, her cancer fight drew a devoted following that reached far beyond her usual country music fans. In December Joey learned that she and Rory had been nominated for a Grammy for their version of “If I Needed You.”
On Feb. 12, the couple released their final album, “Hymns That Are Important To Us,” recorded last summer in Nashville.
Joey passed away yesterday afternoon, surrounded by loved ones:
“My wife’s greatest dream came true today. She is in Heaven.
The cancer is gone, the pain has ceased and all her tears are dry.”
Joey is survived by her almost 2-yr-old daughter Indiana, and two older step-daughters, Heidi and Hopie, from Rory’s previous marriage.
What is the cervix?
The cervix is the lower, narrow end of the uterus (a hollow, pear-shaped organ where a fetus grows). The cervix leads from the uterus to the vagina (birth canal).
In a non-pregnant woman, the cervix is between 2 and 3 cm long and is cylindrical in shape. The lower end of the cervix, called the extocervix, bulges through the front wall of the vagina.
The portion of the cervix between the uterus and the vagina, referred to as the endocervix, is lined with a mucous membrane which contains numerous glands that produce mucus. The extocervix is covered with a scale-like squamous epithelium similar to that of the vagina.
10 Things to Know about Cervical Cancer
- Cervical cancer usually develops slowly over time. Before cancer appears in the cervix, the cells of the cervix go through changes known as dysplasia, in which abnormal cells begin to appear in the cervical tissue. Over time, the abnormal cells may become cancer cells and start to
grow and spread more deeply into the cervix and to surrounding areas. - Infection of the cervix with human papillomavirus (HPV) is almost always the cause of cervical cancer. Not all women with HPV infection, however, will develop cervical cancer. Women who do not regularly have tests to detect HPV or abnormal cells in the cervix are at increased risk of cervical cancer.
- There are usually no signs or symptoms of early cervical cancer but it can be detected early with regular check-ups.
- When symptoms are present, they may include:
- Vaginal bleeding (including bleeding after sexual intercourse).
- Unusual vaginal discharge.
- Pelvic pain.
- Pain during sexual intercourse.
- A pap test and testing for human papilloma virus (HPV) are the most important tests for detecting early cancer and determining risk for cancer.
Pap test: A procedure to collect cells from the surface of the cervix and vagina. A piece of cotton, a brush, or a small wooden stick is used to gently scrape cells from the cervix and vagina. The cells are viewed under a microscope to find out if they are abnormal. This procedure is also called a Pap smear.
Human papillomavirus (HPV) test: A laboratory test used to check DNA or RNA for certain types of HPV infection. Cells are collected from the cervix and DNA or RNA from the cells is checked to find out if an infection is caused by a type of HPV that is linked to cervical cancer.
- After cervical cancer has been diagnosed, tests are done to find out if cancer cells have spread within the cervix or to other parts of the body. This will determine what stage the cancer is.
In stage III, cancer has spread to the lower third of the vagina, and/or onto the pelvic wall, and/or has caused kidney problems.
In stage IV, cancer has spread beyond the pelvis, or can be seen in the lining of the bladder and/or rectum, or has spread to other parts of the body.
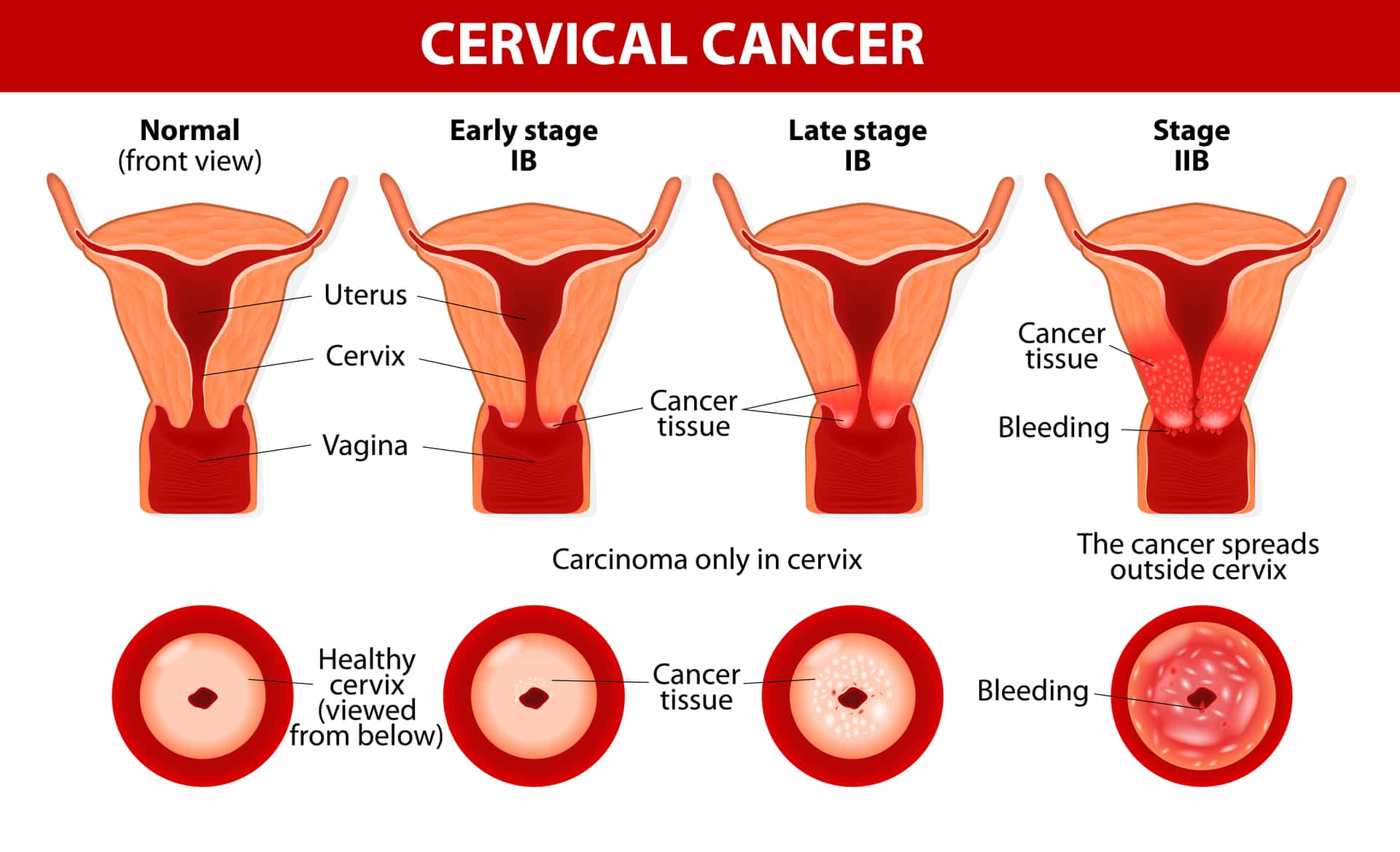
Cervical Cancer. Carcinoma of Cervix. Malignant neoplasm arising from cells in the cervix uteri. Vaginal bleeding. Vector diagram
- Treatment of cervical cancer may include surgery, chemotherapy, radiation therapy, targeted therapy (bevacizumab, AVASTIN®) or a combination of these.
- Conization is a procedure to remove a cone-shaped piece of tissue from the cervix and cervical canal. A pathologist views the tissue under a microscope to look for cancer cells. Conization may be used to diagnose or treat a cervical condition. This procedure is also called a cone biopsy.
- Total hysterectomy is surgery to remove the uterus, including the cervix. In a radical hysterectomy a surgeon removes the uterus, cervix, part of the vagina, as well as a wide area of ligaments and tissues around these organs. The ovaries, fallopian tubes, or nearby lymph nodes may also be removed.
- Vaccines that protect against HPV infection greatly reduce the risk of cervical cancer. These vaccines do not protect women who are already infected with HPV.
The Food and Drug Administration (FDA) has approved two HPV vaccines: Gardasil® for the prevention of cervical, anal, vulvar and vaginal cancer and and Cervarix® for the prevention of cervical cancer and precancerous cervical lesions caused by HPV infection. The vaccines are given through a series of three injections over a 6-month period.
These vaccines are proven to be effective only if given before infection with HPV, so it is recommended that they be given before an individual is sexually active. The Advisory Committee on Immunization Practices (ACIP) recommends:
- Initiation of routine HPV vaccination at age 11 or 12 years (the vaccination series can be started beginning at age 9 years)
- Vaccination of females aged 13 through 26 years and of males aged 13 through 21 years who have not been vaccinated previously or who have not completed the three-dose vaccination series. Males aged 22 through 26 years may be vaccinated.



























0 comments