Lady Gaga Battling Fibromyalgia
Lady Gaga has been forced to cancel the Rio concert of her world tour, citing “severe pain” for which she had to be hospitalized. Gaga wrote on Twitter:
“It’s not simply hip pain or wear & tear from tour, I’m in severe pain. I’m in good hands [with] the very best doctors.”
Gaga has been dealing with a chronic condition called fibromyalgia, which is characterized by severe, widespread pain. In November she posted a description of the ice baths, infrared saunas and emergency blankets she uses to manage her condition.
Her battle with the disease will be featured in an upcoming Netflix documentary Gaga: Five Foot Two. She hopes the documentary will “help raise awareness & connect people who have it.”
What Is Fibromyalgia?
Fibromyalgia syndrome is a common and chronic disorder characterized by widespread pain, diffuse tenderness, and a number of other symptoms. The word “fibromyalgia” comes from the Latin term for fibrous tissue (fibro) and the Greek ones for muscle (myo) and pain (algia).
Although fibromyalgia is often considered an arthritis-related condition, it is not truly a form of arthritis (a disease of the joints). This is because it does not cause inflammation or damage to the joints, muscles, or other tissues. Like arthritis, however, fibromyalgia can cause significant pain and fatigue, and it can interfere with a person’s ability to carry on daily activities. Also like arthritis, fibromyalgia is considered a rheumatic condition, a medical condition that impairs the joints and/or soft tissues and causes chronic pain.
 What are the Symptoms?
What are the Symptoms?
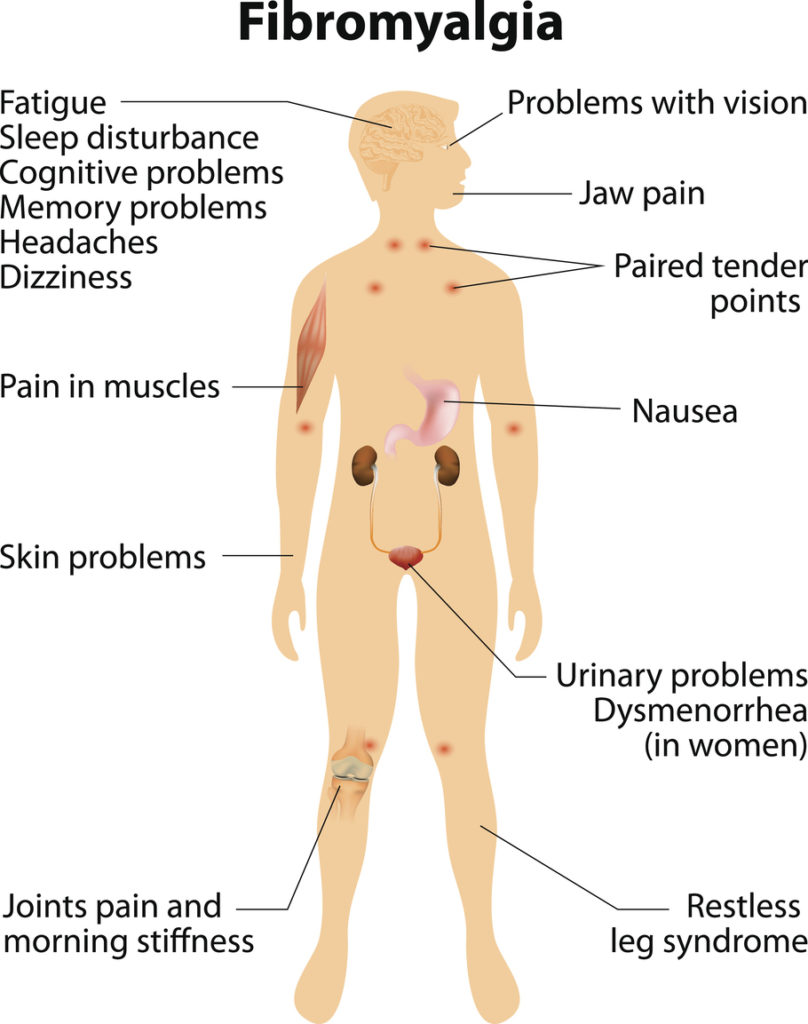
In addition to pain and fatigue, people who have fibromyalgia may experience a variety of other symptoms including:
- cognitive and memory problems (sometimes referred to as “fibro fog”)
- sleep disturbances
- morning stiffness
- headaches
- irritable bowel syndrome
- painful menstrual periods
- numbness or tingling of the extremities
- restless legs syndrome
- temperature sensitivitysensitivity to loud noises or bright lights
A person may have two or more coexisting chronic pain conditions. Such conditions can include chronic fatigue syndrome, endometriosis, fibromyalgia, inflammatory bowel disease, interstitial cystitis, temporomandibular joint dysfunction, and vulvodynia. It is not known whether these disorders share a common cause.
Who Gets Fibromyalgia?
Scientists estimate that fibromyalgia affects 5 million Americans age 18 or older. For unknown reasons, between 80 and 90 percent of those diagnosed with fibromyalgia are women; however, men and children also can be affected. Most people are diagnosed during middle age, although the symptoms often become present earlier in life.
People with certain rheumatic diseases, such as rheumatoid arthritis, systemic lupus erythematosus (commonly called lupus), or ankylosing spondylitis (spinal arthritis) may be more likely to have fibromyalgia, too.
Several studies indicate that women who have a family member with fibromyalgia are more likely to have fibromyalgia themselves. The exact reason for this—whether it is heredity, shared environmental factors, or both—is unknown. Researchers are studying whether variations in certain genes cause some people to be more sensitive to stimuli, which lead to pain syndromes.
What Causes Fibromyalgia?
The causes of fibromyalgia are unknown, but there are probably a number of factors involved. Many people associate the development of fibromyalgia with a physically or emotionally stressful or traumatic event, such as an automobile accident. Some connect it to repetitive injuries. Others link it to an illness. For others, fibromyalgia seems to occur spontaneously.
Many researchers are examining other causes, including problems with how the central nervous system (the brain and spinal cord) processes pain.
Some scientists speculate that a person’s genes may regulate the way his or her body processes painful stimuli. According to this theory, people with fibromyalgia may have a gene or genes that cause them to react strongly to stimuli that most people would not perceive as painful. There have already been several genes identified that occur more commonly in fibromyalgia patients, and NIAMS (National Institute of Arthritis and Musculoskeletal and Skin Diseases)-supported researchers are currently looking at other possibilities.
How Is Fibromyalgia Diagnosed?
Research shows that people with fibromyalgia typically see many doctors before receiving the diagnosis. One reason for this may be that pain and fatigue, the main symptoms of fibromyalgia, overlap with those of many other conditions. Therefore, doctors often have to rule out other potential causes of these symptoms before making a diagnosis of fibromyalgia. Another reason is that there are currently no diagnostic laboratory tests for fibromyalgia; standard laboratory tests fail to reveal a physiologic reason for pain. Because there is no generally accepted, objective test for fibromyalgia, some doctors unfortunately may conclude a patient’s pain is not real, or they may tell the patient there is little they can do.
A doctor familiar with fibromyalgia, however, can make a diagnosis based on criteria established by the American College of Rheumatology (ACR): a history of widespread pain lasting more than 3 months, and other general physical symptoms including fatigue, waking unrefreshed, and cognitive (memory or thought) problems. In making the diagnosis, doctors consider the number of areas throughout the body in which the patient has had pain in the past week.
How Is Fibromyalgia Treated?
Fibromyalgia can be difficult to treat. Not all doctors are familiar with fibromyalgia and its treatment, so it is important to find a doctor who is. Many family physicians, general internists, or rheumatologists (doctors who specialize in arthritis and other conditions that affect the joints or soft tissues) can treat fibromyalgia.
Only three medications, duloxetine, milnacipran, and pregabalin are approved by the U.S. Food and Drug Administration (FDA) for the treatment of fibromyalgia. Duloxetine (Cymbalta) was originally developed for and is still used to treat depression. Milnacipran (Savella) is similar to a drug used to treat depression but is FDA approved only for fibromyalgia. Pregaballin (Lyrica) is a medication developed to treat neuropathic pain (chronic pain caused by damage to the nervous system).
Doctors also treat fibromyalgia with a variety of other medications developed and approved for other purposes. Many people with fibromyalgia also report varying degrees of success with complementary and alternative therapies, including massage, movement therapies (such as Pilates and the Feldenkrais method), chiropractic treatments, acupuncture, and various herbs and dietary supplements for different fibromyalgia symptoms.
Will Fibromyalgia Get Better With Time?
Fibromyalgia is a chronic condition, meaning it lasts a long time—possibly a lifetime. However, it may be comforting to know that fibromyalgia is not a progressive disease. It is never fatal, and it will not cause damage to the joints, muscles, or internal organs. In many people, the condition does improve over time.
What Can I Do to Try to Feel Better?
Besides taking medicine prescribed by your doctor, there are many things you can do to minimize the impact of fibromyalgia on your life. These include:
Getting enough sleep. Getting enough sleep and the right kind of sleep can help ease the pain and fatigue of fibromyalgia (see “Tips for Good Sleep”). Even so, many people with fibromyalgia have problems such as pain, restless legs syndrome, or brainwave irregularities that interfere with restful sleep. It is important to discuss any sleep problems with your doctor, who can prescribe or recommend treatment for them.
Exercising. Although pain and fatigue may make exercise and daily activities difficult, it is crucial to be as physically active as possible. Research has repeatedly shown that regular exercise is one of the most effective treatments for fibromyalgia. People who have too much pain or fatigue to do vigorous exercise should begin with walking or other gentle exercise and build their endurance and intensity slowly.
Making changes at work. Most people with fibromyalgia continue to work, but they may have to make big changes to do so. For example, some people cut down the number of hours they work. Some switch to a less demanding job, or adapt a current job. If you face obstacles at work, such as an uncomfortable desk chair that leaves your back aching or difficulty lifting heavy boxes or files, your employer may make adaptations that will enable you to keep your job. An occupational therapist can help you design a more comfortable workstation or find more efficient and less painful ways to lift.
Eating well. Although some people with fibromyalgia report feeling better when they eat or avoid certain foods, no specific diet has been proven to influence fibromyalgia. Of course, it is important to have a healthy, balanced diet. Not only will proper nutrition give you more energy and make you generally feel better, it will also help you avoid other health problems.
Source: NIAMS



























2 Comments